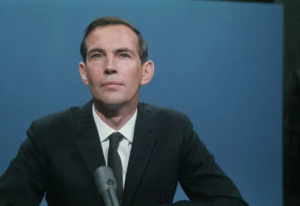
Anthony Fauci Pandemic Leadership Explained
Anthony Fauci: The Human Face of Science in a Pandemic Crisis
Anthony Fauci: The Unlikely Icon

On an unremarkable graduation day at Ohio Stadium, a young Alyse Krauskopf wondered about the “unexciting” commencement speaker—Dr. Anthony Fauci. Four years later, that same man would become America’s scientific compass during its worst health crisis in a century. Born to a Brooklyn pharmacist, delivering prescriptions by bicycle, Fauci’s journey from neighborhood pharmacies to the White House briefing room embodies an extraordinary collision of scientific rigor and human-centered leadership. His story reveals how science survives—and thrives—when clothed in empathy, transparency, and relentless adaptation.
The Science of Preparedness – Lessons Forged in Crisis
The Unseen Foundation of Pandemic Response
When COVID-19 emerged, the world marveled at mRNA vaccines developed in 11 months—a process that historically took decades (47 years for polio, 10 for measles). This “overnight” miracle, Fauci stressed, was built on decades of uncelebrated basic science. “It was all due to things scientists were doing in their lab 15 or 20 years ago without having an obvious pandemic in mind,” he told Cornell audiences in 2023. Yet this triumph highlighted a grim irony: even as vaccines prevented ~3.25 million U.S. deaths, pandemic preparedness funding evaporated once the immediate threat faded. “Corporate memory is fleeting,” Fauci warned—a pattern risking future catastrophes.
Zoonotic Vigilance and the “Wet Market” Nexus
Fauci consistently linked human health to ecological systems. With 75% of emerging infections originating in animals, he identified wildlife trade regulation as critical prevention. While SARS-CoV-2’s origins remain debated, he noted compelling evidence pointing to Wuhan’s wet markets: “Recent data about the mix of DNA from animals with the RNA of the virus makes that more compelling”. This zoonotic lens reframed pandemics not as freak events, but predictable outcomes of human-animal-environment interactions.
The Infrastructure Lifeline: Local Public Health
Among Fauci’s sharpest COVID lessons was the decay of U.S. public health infrastructure. Contact tracing faltered early because local agencies—starved by attrition and underfunding—lacked personnel. “It wasn’t that people were inadequate; there weren’t enough of them,” he observed. His prescription: sustained investment in local response networks between crises—a “perpetual preparedness” ethos.
The Art of Science Communication – Anthony Fauci
Knowing the Audience: From Fox News to The Daily Show
Fauci grasped early that “the American people” were not monolithic. Traditional media (CNN, MSNBC) reached only ~4% of citizens. So he met diverse audiences where they lived: Instagram Live with Stephen Curry, podcasts with Trevor Noah, even YouTube interviews. “We can reach diverse audiences by using social media tools,” he advised scientists—a call to abandon academic isolation for cultural engagement.
Anthony Fauci Golden Rules: Clarity
Fauci distilled scientific communication into three pillars:
- Know your audience
- Limit core messages (1–2 per interaction)
- Prioritize comprehension over intellect
His interviews followed a rhythmic cadence: What we know → What we don’t know → What we should do. This structure resisted the “and… and… and” data dump, focusing instead on actionable insights. When politics intruded, he deflected blame games with “Okay, let’s stop this nonsense,” returning always to evidence.
Empathy as Antidote to Alienation
Fauci’s genius lay in acknowledging hardship before prescribing sacrifice. “Staying home and wearing masks are inconvenient,” he told Steph Curry, “but these actions will allow us to get back to activities we enjoy sooner”. This empathy resonated powerfully—turning him into an unlikely Gen Z meme icon and inspiring viral #MaskUp campaigns. His humanity dissolved barriers: “He spoke to us as equals,” recalled Krauskopf, despite his stature.
| Challenge | Tactic | Example |
|---|---|---|
| Vaccine hesitancy | Trusted messengers resembling audiences | Surgeon General Jerome Adams addressing “Black and Brown sisters and brothers” |
| Misinformation | Flooding the zone with truth | Refusing to “legally suppress” deniers while saturating media with facts |
| Evolving guidance | Transparent self-correction | Explaining mask guidance shifts using new data on asymptomatic spread |
Anthony Fauci Shadow of History – AIDS
“I Was Created for This Disease”: The AIDS Crucible
Fauci’s COVID responses were honed in the AIDS pandemic. “I’m board certified in infectious disease. I’m board certified in immunology. And I’m a practicing immunosuppressive guy,” he reflected. “It was like I was created for this disease”. His early HIV work revealed parallels: stigma, scientific uncertainty, and political neglect. But COVID diverged tragically in its “incredible divisiveness,” whereas AIDS activism ultimately unified communities.
ACT UP and the Democratization of Science

Fauci’s most radical move was embracing AIDS activists like ACT UP—once protesters chaining themselves to NIH gates. Instead of dismissing them, he listened: “Put myself in their shoes… I would do exactly what they did”. This led to transformative changes:
- Patient advocates embedded in drug trial committees
- Approval timelines slashed from 10 years to <1 year
- Placebo trial reforms protecting vulnerable subjects
These innovations later spread to cancer and Alzheimer’s research, proving that “well-informed activists have a major impact on the scientific agenda”.
PEPFAR: The Blueprint for Global Equity
Fauci helped design PEPFAR under George W. Bush—an initiative delivering antiretrovirals to 13.3 million people and averting 2.2 million perinatal HIV infections. This model framed health justice as moral imperative: “We have a moral obligation to not have people die unnecessarily because of where they live”. He later championed COVID vaccine equity using identical logic, urging rich nations to fund global distribution.
Navigating the Misinformation Pandemic
The Enemy of Pandemic Control: False Equivalency
Fauci identified “false equivalency”—treating baseless opinions as equal to evidence—as particularly toxic. During COVID, this manifested as “debates” pitting peer-reviewed science against conspiracy theories. “Social media communication is often with no data, nobody quality controlling it,” he lamented, distinguishing it from rigorous journalism.
Mask Flip-Flops and the Science of Self-Correction
Attacks accusing Fauci of “lying” about masks ignored science’s iterative nature. He unpacked the evolution:
- Initial PPE shortages prioritized healthcare workers
- No pre-COVID data on community mask efficacy
- Game-changing revelations of asymptomatic transmission (50%+ of cases)
“You’ve got to evolve with the science,” he insisted. “Science is a self-correcting process”. This intellectual honesty—admitting “if I knew then what I know now”—became his shield against disingenuous criticism.
Celebrity vs. Scientist: The Personal Toll
Despite viral fame (memes, bobbleheads), Fauci rejected celebrity: “I am fundamentally a scientist.” The adulation carried venom: death threats, partisan vilification, and distortions alleging lab-leak conspiracies. “The same institute they’re attacking… developed the vaccine saving millions,” he noted with anguish. Yet he leveraged visibility for good—exemplifying Alda’s #Vaccie idea by publicly receiving boosters.
The Unfinished Agenda – Equity and Infrastructure
Vaccines and the “Historic Mistrust” Dilemma
COVID exposed fault lines in scientific trust, particularly among communities of color. Fauci and actor Alan Alda stressed tailored outreach: messengers resembling audiences (e.g., Black physicians), non-condescending dialogue, and acknowledging historical abuses like Tuskegee. Jerome Adams’ video—“Black and Brown sisters and brothers”—modeled this.
Anthony Fauci Public Health’s Backbone
The pandemic’s structural lesson was clear: local health departments needed reinforcements before emergencies. Fauci urged sustained funding to reverse attrition—a “perpetual preparedness” mantra extending beyond labs to frontline responders.
| Pandemic | Core Challenge | Fauci’s Innovation | Legacy |
|---|---|---|---|
| AIDS | Stigma, slow drug approvals | Partnering with activists; accelerated trials | Patient advocates in research; global PEPFAR program |
| COVID-19 | Misinformation; polarization | Cross-platform science communication; adapting guidance | Blueprint for rapid vaccine development; equity frameworks |
| Future Threats | Preparedness funding cycles | “Durable corporate memory” advocacy | Infrastructure investment; zoonotic surveillance |
Anthony Fauci: “Science Will Save Us” –Faith
In December 2020, as vaccines rolled out, Fauci declared to Alan Alda: “When this is over… we’ll look back and say, ‘It was science that got us out of this, pure science’”. This conviction—forged across pandemics—anchored his legacy. Yet his true achievement was humanizing that science: listening to AIDS protesters, explaining masks to frightened families, and acknowledging uncertainty without surrendering authority.
As museums now collect COVID artifacts—vial empties, ventilator prototypes—they preserve more than objects. They enshrine a principle Fauci embodied: that science, divorced from empathy, communication, and justice, cannot heal. In a divided world, his career whispers a persistent truth: Viruses need not be partisan. The enemy is complacency, not each other. And the cure—always—is shared humanity.
“You can address a perpetual challenge by being perpetually prepared. To me, that’s the overarching message.”